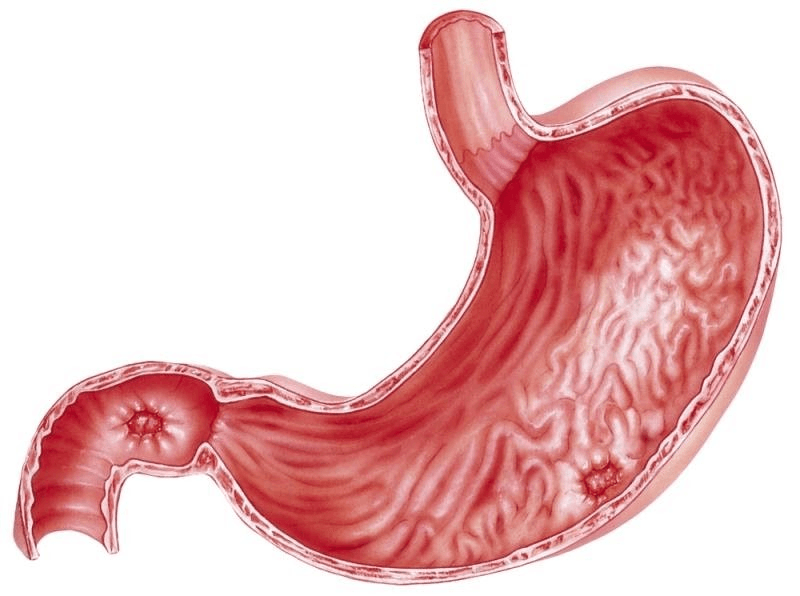
The stomach is protected by a mucus layer called the gastric mucosa. This mucous lining shields the stomach from the harsh effects of gastric acid, which helps digest food. When this protective layer is damaged or weakened by various factors, the mucosa becomes inflamed, irritated, or eroded, leading to gastritis (stomach inflammation). Similarly, duodenitis is inflammation of the duodenal mucosa, the first part of the small intestine located just below the stomach. Both gastritis and duodenitis share similar causes and treatment approaches.
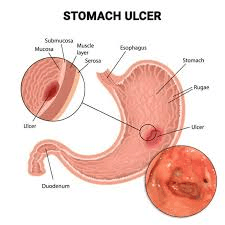
Symptoms of Gastric and Duodenal Ulcers
Gastric and duodenal ulcers are common digestive conditions affecting both men and women across all ages. These conditions can be acute, developing suddenly and lasting for a short period, or chronic, progressing slowly and persisting for months or even years. Generally, these ulcers can be treated effectively without causing long-term complications.
Risk Factors for Gastric and Duodenal Ulcers
Certain groups of people, such as the elderly and those with weakened immune systems, are more prone to developing gastric and duodenal ulcers. Other health conditions and lifestyle factors also increase the risk. Smoking, high stress levels from work or life, excessive use of stimulants like alcohol or cocaine, chronic vomiting, and vitamin B12 deficiency are some of the contributing factors. Additionally, frequent use of NSAIDs (nonsteroidal anti-inflammatory drugs), corticosteroids, exposure to radiation, autoimmune diseases such as Hashimoto’s thyroiditis or type 1 diabetes, infections like tuberculosis and syphilis, and Helicobacter pylori infection all play important roles in the development of ulcers.
Causes of Gastric and Duodenal Ulcers
The most common cause of gastritis and duodenitis is infection by the bacterium Helicobacter pylori (H. pylori). When this bacteria colonizes the stomach or duodenum in large numbers, it causes inflammation. H. pylori can spread from person to person, most likely through contaminated food or water. Other causes include long-term use of NSAIDs or corticosteroids, excessive alcohol consumption, autoimmune disorders, celiac disease, bile reflux, and infections from other bacteria or viruses such as Mycobacterium avium-intracellulare, herpes simplex virus, and cytomegalovirus. Parasitic infections and physical injuries to the stomach or intestines, as well as treatments like chemotherapy, radiation, and mechanical ventilation, can also contribute to inflammation.
Symptoms and Signs of Gastric and Duodenal Ulcers
Not all cases of gastritis or duodenitis cause symptoms; sometimes, the condition is discovered incidentally during investigations for other digestive problems. When symptoms do occur, they often include a burning or painful sensation in the stomach, nausea, vomiting, indigestion, feeling full quickly even after eating small amounts, and pain radiating to the back or lower abdomen. These symptoms can vary in intensity and frequency depending on whether the condition is acute or chronic.
Severe Symptoms That Require Immediate Medical Attention
Severe symptoms of gastric and duodenal ulcers may include shortness of breath, chest pain, vomiting blood, intense abdominal pain, foul-smelling stools, rapid heartbeat, excessive sweating, fever, and signs of bleeding such as black or tarry stools. These signs require urgent medical care.
Diagnosis of Gastric and Duodenal Ulcers
Doctors typically diagnose ulcers based on patient history and physical exams but may order additional tests to confirm the diagnosis and identify the cause. Common diagnostic tools include tests for H. pylori infection through breath or stool samples, upper gastrointestinal endoscopy to visually inspect the stomach and duodenum and to take biopsy samples, and barium X-rays to identify ulcer locations. Blood tests to check organ function, anemia, or infections might also be necessary.
Complications of Gastric and Duodenal Ulcers
Chronic gastritis can increase the risk of developing stomach ulcers and bleeding. Certain types of gastritis, including autoimmune gastritis and H. pylori-induced gastritis, may impair the body’s ability to absorb iron and vitamin B12, potentially leading to anemia. Moreover, H. pylori infection slightly raises the risk of stomach cancer, underscoring the importance of early detection and treatment.
Prevention and Lifestyle Recommendations
Many healthcare providers recommend lifestyle changes to reduce inflammation and support healing in the stomach and duodenum. Avoiding or limiting alcohol and tobacco use helps reduce irritation and promote tissue repair. Medications such as NSAIDs and aspirin, which increase ulcer risk, should be used cautiously and under medical guidance. For those who need to use these medications long-term, doctors might suggest lower doses or alternative drugs to minimize stomach damage. People with gluten intolerance or celiac disease need to avoid gluten to prevent inflammation.
Conclusion
Gastric and duodenal ulcers are manageable conditions that benefit greatly from timely diagnosis and appropriate treatment. Understanding risk factors, recognizing symptoms early, and following medical advice can prevent serious complications. Adopting healthy lifestyle habits, including avoiding irritants and maintaining a balanced diet, also plays a crucial role in ulcer prevention and recovery.
For those looking to support their digestive health naturally, Stomach Saviour – Fix Your Gut Fast and Forever offers a convenient audio program designed to guide you through effective, gentle strategies to promote gut balance and comfort. This downloadable audiobook provides practical advice and soothing techniques that complement medical treatments and lifestyle adjustments, helping you take positive steps toward lasting digestive wellness. Always remember to consult your healthcare provider to ensure any new approach fits your individual needs.